Introduction
As a woman approaching or going through menopause, it is essential to understand the impact it can have on your bone health. During this stage of life, hormonal changes can increase the risk of osteoporosis, a condition characterized by weak and brittle bones. In this blog post, we will explore how menopause influences bone health and the connection between menopause and osteoporosis.
Menopause and its impact on bone health
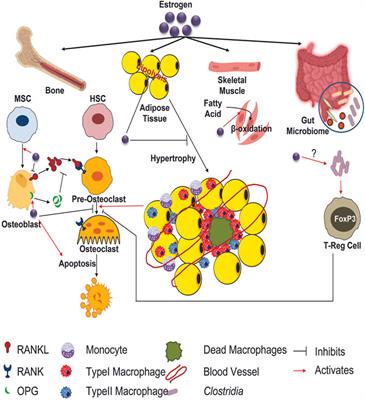
During menopause, your body experiences a significant decline in estrogen levels. Estrogen plays a crucial role in maintaining bone density and strength. When these estrogen levels drop, it can lead to bone loss and an increased risk of developing osteoporosis. The decreased estrogen levels can affect the balance between bone breakdown and formation, resulting in a higher rate of bone resorption.
Additionally, menopause often coincides with aging, which is another factor that contributes to bone loss. As you age, your body may become less efficient at absorbing and metabolizing calcium, a key mineral for bone health. This can further exacerbate the effects of menopause on bone density.
Understanding the connection between menopause and osteoporosis
Osteoporosis is a condition characterized by low bone mass, which leads to fragile and brittle bones. It is common for women to develop osteoporosis during and after menopause due to the hormonal changes mentioned earlier. The decrease in estrogen levels, along with other factors such as age, genetics, and lifestyle choices, can significantly increase the risk of developing osteoporosis.
It is crucial for women going through menopause to prioritize their bone health. This can be done through various strategies such as regular weight-bearing exercises, a balanced diet rich in calcium and vitamin D, and lifestyle modifications like avoiding smoking and excessive alcohol consumption.
By understanding the connection between menopause and osteoporosis, you can take proactive steps to protect your bone health. Regular check-ups with your healthcare provider and discussing any concerns or risk factors related to osteoporosis are crucial for early detection and prevention of this condition. Remember, your bone health is important, and taking care of it during and after menopause will help ensure a strong and healthy future.

Hormonal Changes and Bone Loss
Role of estrogen in maintaining bone density
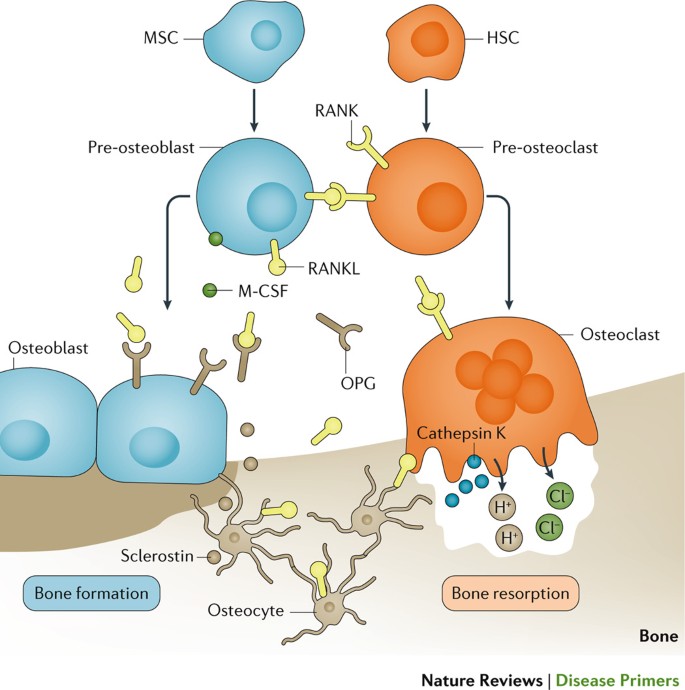
During your reproductive years, estrogen plays a vital role in maintaining bone density and strength. It helps to regulate the balance between bone breakdown and formation, ensuring that your bones stay healthy and strong. Estrogen promotes the activity of bone-building cells called osteoblasts, while also reducing the activity of bone-resorbing cells called osteoclasts. This balance ensures that new bone is constantly being formed to replace older bone.
Effects of declining estrogen levels on bone health
As you approach menopause, the levels of estrogen in your body begin to decline. This decrease in estrogen can have a significant impact on your bone health. Without adequate estrogen, the balance between bone breakdown and formation is disrupted, leading to bone loss. The rate of bone resorption, or breakdown, starts to exceed the rate of bone formation, resulting in a gradual loss of bone density and strength.
The decline in estrogen levels also coincides with the natural aging process, which further contributes to bone loss. As you age, your body becomes less efficient at absorbing and utilizing calcium, a mineral essential for bone health. This reduction in calcium absorption, coupled with decreased estrogen levels, accelerates the rate of bone loss and increases the risk of osteoporosis.
It is important to understand the connection between menopause and bone health so that you can take proactive steps to protect your bones. Regular weight-bearing exercises, such as walking or dancing, can help to maintain bone density. A balanced diet rich in calcium and vitamin D, which aids calcium absorption, is also crucial. Additionally, avoiding smoking and excessive alcohol consumption can further protect your bones.
By understanding the impact of menopause on bone health and taking preventive measures, you can reduce the risk of osteoporosis and ensure that your bones remain strong and healthy. Consult with your healthcare provider to discuss any concerns or risk factors related to osteoporosis and develop a personalized plan to support your bone health during and after menopause.
Understanding Bone and Joint Inflammation: Causes, Symptoms, and Treatments
Hip replacement: A surgical procedure that involves replacing a damaged hip joint with an artificial one
Promising Research and Developments for Rheumatoid Arthritis Treatments
Rheumatoid Arthritis in Children: Signs, Symptoms, and Treatment
Overcoming Fatigue and Depression Associated with Rheumatoid Arthritis
The Relationship Between Diet and Rheumatoid Arthritis Management
When to Seek Medical Help for Rheumatoid Arthritis
Key Differences Between Rheumatoid Arthritis and Osteoarthritis
Living with Rheumatoid Arthritis: Coping Strategies and Treatment Options
Understanding the Symptoms and Causes of Rheumatoid Arthritis
Decreased Calcium Absorption
How menopause affects calcium absorption
During menopause, hormonal changes can significantly impact your body's ability to absorb and utilize calcium. Estrogen, which plays a crucial role in bone health, decreases as you go through menopause. This decline in estrogen levels directly affects calcium absorption in your body.
Calcium absorption occurs primarily in the small intestine. Estrogen supports the production of a hormone called calcitriol, which helps increase calcium absorption. However, with lower estrogen levels, the production of calcitriol is reduced, leading to decreased calcium absorption.
Impact of calcium deficiency on bone strength
Diminished calcium absorption during menopause can have severe implications for your bone health. Calcium is a fundamental mineral that provides strength and structure to your bones. Calcium deficiency can weaken your bones, making them more susceptible to fractures and osteoporosis.
Osteoporosis is a condition characterized by the loss of bone mass and density. It increases the risk of fractures, particularly in the hips, wrists, and spine. Calcium deficiency, coupled with declining estrogen levels, accelerates the rate of bone loss and heightens the risk of developing osteoporosis during menopause.
To mitigate the impact of decreased calcium absorption and reduce the risk of osteoporosis, it is essential to prioritize calcium-rich foods in your diet. Dairy products like milk, cheese, and yogurt are excellent sources of calcium. Additionally, leafy green vegetables, fortified cereals, and tofu can contribute to your calcium intake.
Supplementation may also be necessary to meet your calcium requirements. Consult with your healthcare provider to determine the appropriate dosage and discuss any potential interactions with other medications.
By addressing the decreased calcium absorption during menopause, you can support your bone health and minimize the risk of developing osteoporosis. Prioritize calcium-rich foods and consider supplementation to ensure your body receives adequate calcium for maintaining strong and healthy bones.
Accelerated Bone Loss
Increased bone resorption during menopause
During menopause, hormonal changes can lead to an acceleration of bone loss in your body. As estrogen levels decline, bone resorption, the process of breaking down old bone tissue, starts to outpace bone formation. This imbalance can result in a significant loss of bone density and strength.
The decline in estrogen levels directly affects bone cells known as osteoclasts, which are responsible for breaking down old bone tissue. With lower estrogen levels, the activity of osteoclasts increases, leading to excessive bone resorption. This heightened bone resorption contributes to the overall loss of bone mass during menopause.
Reduced bone formation and its consequences
Alongside increased bone resorption, reduced bone formation during menopause further exacerbates bone loss. Estrogen plays a vital role in the process of bone formation by promoting the activity of bone-building cells called osteoblasts. With decreased estrogen levels, the production and activity of osteoblasts decrease, impairing the body's ability to build new bone tissue.
The combination of increased bone resorption and reduced bone formation results in a significant decrease in bone density. As bone density decreases, your bones become weaker and more susceptible to fractures. This increased fragility puts you at a higher risk of developing osteoporosis, a condition characterized by weak and brittle bones.
To combat accelerated bone loss during menopause and reduce the risk of osteoporosis, several strategies can be employed. Regular weight-bearing exercises such as walking, jogging, and resistance training can help stimulate bone formation. Ensuring an adequate intake of calcium and vitamin D, either through dietary sources or supplementation, is also crucial for maintaining bone health.
Additionally, it is important to consult with your healthcare provider to assess your individual bone health and determine if any additional interventions, such as hormone replacement therapy or medication, may be necessary to support your bone density.
By addressing the accelerated bone loss that occurs during menopause, you can take proactive steps to protect your bone health and reduce the risk of osteoporosis. Prioritizing exercise, calcium-rich foods, and appropriate supplementation can support your bones and maintain their strength throughout this stage of life.
Menopausal Symptoms and Bone Health
Relationship between menopausal symptoms and bone health
Menopause brings about a range of symptoms due to hormonal changes in the body, and these symptoms can have an impact on your bone health. The decline in estrogen levels during menopause not only affects the reproductive system but also plays a significant role in bone health. Estrogen is essential for maintaining bone density and strength, so when its levels decrease, the risk of bone loss increases.
Effects of hot flashes, night sweats, and sleep disturbances on bones
Hot flashes, night sweats, and sleep disturbances are common symptoms experienced during menopause. These symptoms can disrupt your sleep patterns, leading to inadequate rest and negatively impacting bone health. Quality sleep is crucial for the repair and regeneration of bones and other tissues. When you're consistently not getting enough sleep due to hot flashes and night sweats, it can hinder the body's ability to properly maintain and strengthen bones.
This disruption in sleep patterns can contribute to increased bone loss and further exacerbate the risk of osteoporosis. Studies have shown that women experiencing frequent and severe hot flashes during menopause are more likely to have lower bone mineral density.
It is important to address these menopausal symptoms and their impact on bone health. Seeking medical advice from a healthcare professional can help identify appropriate strategies to manage hot flashes, night sweats, and sleep disturbances. Hormone replacement therapy (HRT) is one possible solution that can help alleviate these symptoms and potentially minimize bone loss.
Additionally, practicing good sleep hygiene, such as creating a comfortable sleep environment and establishing a consistent bedtime routine, may help improve sleep quality. Engaging in stress-reduction techniques, such as relaxation exercises or meditation, can also aid in managing symptoms and promoting better sleep.
By recognizing the relationship between menopausal symptoms and bone health, you can take proactive steps to manage these symptoms and reduce the impact on your bones. Prioritizing sleep and seeking appropriate medical guidance can play a crucial role in maintaining bone density and reducing the risk of osteoporosis during menopause.